Researchers Find More Harm Than Good in This Widely Recommended Preventive Screen
The controversy and debate seem unending. They tell you to take these studies with a grain of salt. But evidence of harm keeps piling up. And even though Congress ordered insurance to pay up for it, you'll want to get the facts and proceed with caution. Your life could be on the line.
October 25, 2016
Story at-a-glance
- Mammography has many drawbacks, including false positives, false negatives, the use of ionizing radiation, which can cause cancer, and the fact that mammograms have no apparent impact on mortality rates
- Mammograms are said to reduce your risk of dying from breast cancer by 20 percent, but in reality, this amounts to 1 woman’s life being saved out of 1,000 women who get regular mammograms over a lifetime
- A recent study again refutes the use of mammography as a primary tool for cancer prevention, as it has no impact on mortality rates and harms more women than it helps
By Dr. Mercola
I've written many articles on the hazards and drawbacks of mammograms, which include:
•The risk of false positives. Besides leading to unnecessary mental anguish and medical treatment, a false cancer diagnosis may also interfere with your eligibility for medical insurance, which can have serious financial ramifications
•The risk of false negatives, which is of particular concern for dense-breasted women
•The fact that ionizing radiation actually causes cancer and may contribute to breast cancer when done over a lifetime.
Results published in the British Medical Journal (BMJ) show that women carrying the BRCA1/2 gene mutation are particularly vulnerable to radiation-induced cancer1
•The fact that studies repeatedly find that mammograms have no impact on mortality rates
As so expertly demonstrated in the video above, created by Dr. Andrew Lazris and environmental scientist, Erik Rifkin, Ph.D., it's easy to misunderstand the benefits of mammograms.
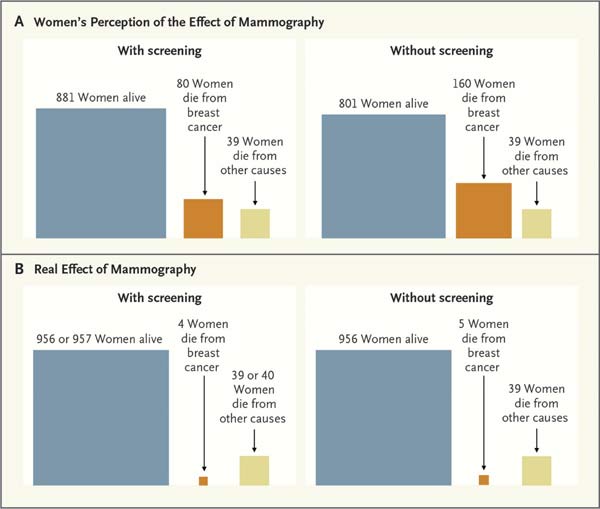
Mammograms are said to reduce your risk of dying from breast cancer by 20 percent, but unless you understand where this number comes from, you'll be vastly overestimating the potential benefit of regular mammogram screening.
Most doctors also fail to inform patients about the other side of the equation, which is that far more women are actually harmed by the procedure than benefit from it.
1 in 1,000 Women Is Saved by Regular Mammogram Screening While 10 Undergo Cancer Treatment for No Reason
Incredible as it may sound, the 20 percent mortality risk reduction touted by conventional medicine actually amounts to just 1 woman per 1,000 who get regular mammograms. How can that be?
As explained in the video, for every 1,000 women who do not get mammograms, 5 of them will die of breast cancer. For every 1,000 women who do get mammograms, 4 will die anyway.
The difference between the two groups is 20 percent (the difference of that one person in the mammogram group whose life is saved). On the other side of the equation, out of every 1,000 women who get regular mammograms over a lifetime:
- HALF will receive a false positive. So while they do NOT have cancer, about 500 out of every 1,000 women getting mammograms will face the terror associated with a breast cancer diagnosis
- 64 will get biopsies, which can be painful and carry risks of adverse effects
- 10 will go on to receive cancer treatment for what is in actuality NOT cancer, including disfiguring surgery and toxic drugs or radiation. Surgery, chemo and radiation are all risky, and dying from the treatment for a cancer you do not have is doubly tragic
All things considered, the evidence seems quite clear; most women should probably avoid mammograms, as they cause far more harm than good.
Many studies have now come to that conclusion, and the most recent research,2published just in time for Breast Cancer Awareness Month, again hammers home that point.
Harms of Mammography Eclipse Benefits
For this study, the researchers analyzed U.S. cancer statistics collected by the government in order to estimate the effectiveness of mammography.
By comparing records of breast cancers diagnosed in women over the age of 40 between 1975 and 1979 — a time before mammograms came into routine use — and between 2000 and 2002, three key findings emerged.3,4,5,6,7,8
- The incidence of large tumors (2 centimeters or larger) has declined, from 68 percent to 32 percent
- The number of women diagnosed with small tumors has increased, from 36 to 64 percent
- The incidence of metastatic cancer, which is the most lethal, has remained stable
This may initially sound like good news for mammograms, but in absolute numbers, the decrease in large tumors was actually rather small — a mere 30 tumors less per 100,000 women.
Meanwhile, the dramatic increase in small tumors was mostly attributed to overdiagnosis — an estimated 81 percent of these small tumors did not actually need treatment.
The fact that metastatic cancer rates remained even suggests we're not catching more of them, earlier. Instead, we're catching and treating mostly harmless tumors.
The researchers also found that two-thirds of the reduction in breast cancer mortality was attributable to improved treatment, such as the use of tamoxifen. Breast cancer screening only accounted for one-third of the reduction in mortality.
Lead researcher Dr. H.Gilbert Welch explains the findings of the study in the video above. As reported by WebMD:9
"The upshot, according to Welch, is that mammography is more likely to 'overdiagnose' breast cancer than to catch more-aggressive tumors early. What's more, the researchers said that while breast cancer deaths have fallen since the 1970s, that is mainly due to better treatment — not screening.
Welch noted the current study's findings have nothing to do with women who feel a lump in the breast. 'They need to get a mammogram,' he stressed. But, Welch suggested, when it comes to routine screening, women can decide based on their personal values."
Screening as Personal Choice
When speaking to NBC news, Welch went on to say that "screening is a choice. It's not a public health imperative."10 At present, most conventional cancer specialists do view mammograms as an imperative, although recommendations vary depending on who you listen to.
As of last year, the American Cancer Society (ACS) recommends women of average risk should have their first mammogram at age 45, followed by an annual mammogram up until age 55. Women 55 and older should have them every other year.11
Meanwhile, the U.S. Preventive Services Task Force (USPSTF) recommends waiting until the age of 50, and only getting a mammogram every other year thereafter.12 In response to heated debate over the varying guidelines, the U.S. Congress passed legislation requiring insurance companies to cover mammograms regardless of age.
Not surprisingly, the ACS has sharply criticized the latest study. In a statement, chief cancer control officer of ACS, Dr. Richard Wender, said: "These conclusions are bold, attention-grabbing and should be taken with a grain of salt — actually, an entire spoonful."
The problem with Wender's attitude is that this is by no means the first or only study suggesting that mammography has been vastly oversold. In fact, a number of studies have now refuted the validity of mammography as a primary tool against breast cancer.
The Evidence Overwhelmingly Refutes Routine Use of Mammography
Other studies that support the findings of the featured study include the following:
Archives of Internal Medicine, 2007: A meta-analysis of 117 randomized, controlled mammogram trials. Among its findings: Rates of false-positive results are as high as 56 percent after 10 mammograms.13
|
Cochrane Database Review, 2009: This review found that breast cancer screening led to a 30 percent rate of overdiagnosis and overtreatment, which actually INCREASED the absolute risk of developing cancer by 0.5 percent.
The review concluded that for every 2,000 women invited for screening throughout a 10-year period, the life of just one woman was prolonged, while 10 healthy women were treated unnecessarily.14
|
New England Journal of Medicine (NEJM), 2010: This study concluded that the reduction in mortality as a result of mammographic screening was so small as to be nonexistent — a mere 2.4 deaths per 100,000 person-years were spared as a result of the screening.15
|
The Lancet Oncology, 2011: This study described the natural history of breast cancers detected in the Swedish mammography screening program between 1986 to 1990, involving 650,000 women.
Since breast lesions and tumors are aggressively treated and/or removed before they can be determined with any certainty to be a clear and present threat to health, there has been little to no research on what happens when they are left alone.
This study however, demonstrated for the first time that women who received the most breast screenings had a HIGHER cumulative incidence of invasive breast cancer over the following six years than the control group who received far less screenings.16
|
The Lancet, 2012, showed that for every life saved by mammography screening, three women are overdiagnosed and treated with surgery, radiation or chemotherapy for a cancer that might never have given them trouble in their lifetimes.17
|
Cochrane Database Review, 2013: A review of 10 trials involving more than 600,000 women found mammography screening had no effect on overall mortality.18
|
NEJM, 2014: Drs. Nikola Biller-Andorno and Peter Jüni published a paper in which they describe the findings of an independent health technology assessment initiative to assess the effectiveness of mammography, of which they were a part:19
|
British Medical Journal (BMJ), 2014: A Canadian study put the rate of overdiagnosis and overtreatment from mammography at nearly 22 percent.21
|
JAMA Internal Medicine, July 2015: Here, researchers concluded mammography screenings lead to unnecessary treatments while having virtually no impact on the number of deaths from breast cancer. A positive correlation between breast cancer screening and breast cancer incidence was indeed found, but there was no positive correlation with mortality.22,23
|
Journal of the Royal Society of Medicine, September 2015: The conclusion of this study is stated right in the title, which reads: "Mammography screening is harmful and should be abandoned."24,25
In short, the authors concluded that decades of routine breast cancer screening using mammograms has done nothing to decrease deaths from breast cancer, while causing more than half (52 percent) of all women undergoing the test to be overdiagnosed and overtreated.
According to lead author Peter C. Gøtzsche, had mammograms been a drug, "it would have been withdrawn from the market long ago."
|
It's Time to Revise the 'When in Doubt, Cut It Out' Mentality
Going back to where we started, even when using the cancer industry's own statistics mammography comes up short, provided you understand what the 20 percent actually means. To reiterate, the difference between getting routine mammograms and not getting them is that the life of 1 in 1,000 women is saved.
Four die even with mammograms, compared to five deaths among those who do not get screened. And again, 10 of those 1,000 screened women will be treated for cancer even though they do not actually have it. Clearly the choice is yours. If you find comfort in thinking you may be that one person who is saved, then by all means follow your heart or gut instinct.
Just be clear about the risks, because the chances are far greater you could be one of the 10 who ends up undergoing chemo or a mastectomy for a tumor that would not have caused you harm. As noted by Dr. Joann Elmore of the University of Washington School of Medicine:26
"We get credit for curing disease that never would have harmed the patient. We receive positive feedback from patients thanking us for 'saving my life,' alarming feedback from patients with 'missed diagnoses' and no feedback at all from patients whose cancer was overdiagnosed. The mantras, 'All cancers are life-threatening' and 'When in doubt, cut it out', require revision."
Solid Evidence for Vitamin D as a Cancer Prevention Tool
Mammograms are portrayed as the best form of "prevention" a woman can get. But early diagnosis is not the same as prevention. And when the cancer screening does more harm than good, how can it possibly qualify as your best hope? I believe the evidence really speaks for itself when it comes to mammography.
The same can be said for research into vitamin D, which repeatedly shows that optimizing your vitamin D level within a range of 40 to 60 nanograms per milliliter (ng/ml) provides impressive cancer protection. I believe testing your vitamin D level is one of the most important cancer prevention tests available. Ideally get tested twice a year.
There are exceptions, of course. If you feel a lump in your breast, a mammogram may be warranted, although even then there are other non-ionizing alternatives, such as ultrasound, which has been shown to be considerably superior to mammography, especially for dense-breasted women who are at much higher risk of a false negative when using mammography.
One of the most recent studies27 looking at vitamin D for breast cancer found that vitamin D deficiency is associated with cancer progression and metastasis. As noted by Stanford University researcher, Dr. Brian Feldman:28
"A number of large studies have looked for an association between vitamin D levels and cancer outcomes, and the findings have been mixed. Our study identifies how low levels of vitamin D circulating in the blood may play a mechanistic role in promoting breast cancer growth and metastasis."
Having higher levels of vitamin D has also been linked to increased likelihood of survival after being diagnosed with breast cancer.29 In one study, breast cancer patients who had an average of 30 ng/ml of vitamin D in their blood had a 50 percent lower mortality rate compared to those who had an average of 17 ng/ml of vitamin D.
I am really grateful that the medical community has embraced vitamin D and started using it. However, it's important to understand that the best way to get vitamin D is from sensible sun exposure, and if you're really interested in optimal health and healing you will do everything in your power to get it. This is one of the reasons I moved to Florida. I have not swallowed vitamin D in over 8 years and still have levels over 60 ng/ml.
There are many other benefits of sunlight exposure other than vitamin D. Over 40 percent of sunlight is near-infrared rays that your body requires to structure the water in your body and stimulate mitochondrial repair and regeneration. If you merely swallow vitamin D and avoid the sun, you are missing a primary benefit of sensible sun exposure.
If you are stuck in the winter and have low vitamin D, it is probably best to swallow oral vitamin D like a drug, but please recognize that this is a FAR inferior way to optimize vitamin D levels and you are missing many important biological benefits when you avoid sun exposure.
You can learn more about vitamin D's influence on cancer and other health problems in my previous article, "The Who, Why and When of Vitamin D Screening." The fact of the matter is there are many strategies that are far more beneficial in terms of breast cancer prevention than mammography. So if you're hitching your fate on mammograms, you're doing yourself a huge disservice.
For key dietary guidelines and lifestyle strategies that can help reduce your cancer risk, please see my previous article, "Top Tips to Decrease Your Breast Cancer Risk." Another excellent resource is Dr. Christine Horner's book, "Waking the Warrior Goddess: Dr. Christine Horner's Program to Protect Against and Fight Breast Cancer," which contains scientifically validated all-natural approaches that can protect against and treat breast cancer.