- The extreme lows brought by Covid-19 have sparked unprecedented speed in developing and approving vaccines and rolling them out
- A number of factors beyond the shots themselves will determine if and how transmissions are curbed
It is a record. Before this, no vaccine had been developed in less than four years, sometimes taking decades.
How history was made in 2020
For example, on January 13 last year, US company Moderna and the National Institutes of Health had already finalised the sequence for an mRNA vaccine against the new virus and they soon began to make a clinical batch.
Oxford University also moved quickly to adapt its research on a Middle East respiratory syndrome vaccine using a chimpanzee virus as a vector to express Sars-CoV-2, the official name of the new coronavirus.
“If you asked in February and March [2020] whether we have a vaccine available in December, nobody would have said that is going to happen that quickly,” said John Moore, professor of microbiology and immunology at Weill Cornell Medical College in New York.
But scientific research in vaccines over the past decade laid the groundwork.
“You have to remember the programme did not start from nothing,” Moore said.
For example, even though there has never been an mRNA vaccine for humans, there has been research into the technology for about 10 years, including laboratory and early clinical tests to determine whether it might work to tackle diseases such as Ebola, Zika, influenza and cancer.
In the past, developers needed to make sure the vaccines worked before they could start manufacturing. But now, massive government funding allowed them to invest in manufacturing facilities before they had to prove the vaccines worked.
“There are a couple of reasons that inactivated vaccines are not really pursued in the West. One, is it is an old technology and pharmaceutical companies have moved on to more modern methods,” Moore said.
“The second is that there is always a risk, going back decades ago, of not inactivating vaccines thoroughly enough and leaving some virus around,” he added, referring to an accident in the US in 1955 related to polio vaccines.
He said there was no longer a culture facility in the US suited to making – and inactivating – large amounts of live virus.
China’s approach, however, is paying off. China was never a global leader in vaccine research but it has emerged as a front runner in the Covid-19 vaccine race. This is despite not being the first country to cross the finishing line, hampered by too few local cases for efficacy analysis and forced to host the final phase of vaccine trials in other countries.
Trial and regulatory review procedures were compressed and held simultaneously to speed up the process, which analysts said could be an example for future research.
Stanley Plotkin, who invented the rubella vaccine in the 1960s and was an important player in the vaccine industry for decades, said the scientific events of last year were unprecedented and would change the playbook for vaccine research.
“Never before have so many developers … worked on a single vaccine using so many different platforms in so short a time. Yes, it will help in the future,” Plotkin said.
But the surprisingly fast progress also depends on a bit of luck, as the virus turns out to be less tricky than some other pathogens for vaccine development.
Most of the 63 vaccines now undergoing clinical trials target the spike protein of the coronavirus that binds to human cells. The target, which was identified based on past vaccine research for coronaviruses, turned out to be the right one.
John Moore said: “HIV, for example, is much harder to vaccinate against … Influenza is much harder to deal with than Sars-CoV-2. So Sars-CoV-2 looks like it is quite easy compared to some pathogens. It has the side of vulnerability that can be exploited – that does not apply as much to other viruses.”
What should we expect in 2021?
Uncertainties remain about whether and when the vaccines can bring an end to the pandemic, which infected over 87 million and killed at least 1.8 million people in roughly one year.
Efficacy data from the front-running vaccines are all far better than the benchmark of 50 per cent set by the WHO and regulators in many countries.
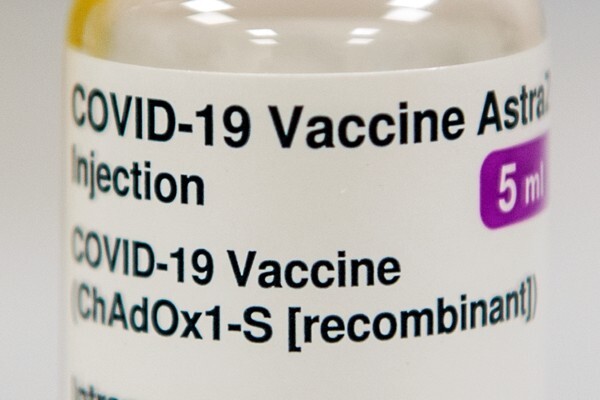
The two mRNA vaccines developed by Pfizer-BioNTech and Moderna achieved about 95 per cent respectively. The vectored vaccine by Oxford-AstraZeneca had an efficacy rate of at least 70 per cent, although it could be even higher after adjusting the dosing.
China also announced one of its inactivated vaccines had an efficacy of 79 per cent. The country gave conditional approval to the vaccine for market launch on December 31 and promised to offer free inoculations to the public. It also has an ambitious plan to vaccinate 50 million people in high-priority groups before the Lunar New Year travel peak in mid-February.
However, the efficacy rates of these vaccines – whose trials compare symptomatic infections in different groups – cannot show how effectively the vaccines stop transmission. There remains scant information about how well the vaccines stop asymptomatic infections. And not all vaccine trials show how well they can protect elderly or seriously ill patients.
Scientists, therefore, will closely monitor whether transmission rates drop in the new year, a factor closely linked to accessibility of the vaccines and the public’s willingness to take the jabs.
“[Experts will be looking for] decreasing hospitalisations, but also decreasing infections indicating decreased spread of the virus,” Plotkin said.
Michael Kinch, director of the Centre for Research Innovation in Biotechnology at Washington University in St Louis, said the duration of protection and virus mutation would determine if the vaccines could really end the pandemic.
“Evidence is mounting that natural infection – becoming sick from the virus – may not provide durable immunity in some. The key is whether a vaccine might overcome this limitation,” he said.
So far, the new variant discovered in London, although rendering the virus more transmissible, does not affect the spike protein targeted by the vaccines, but mutations that could potentially appear in the coming year will affect the success of inoculation programmes.
Safety issues – ranging from long-term and rare side effects, production quality and human errors in inoculation – can also pose challenges. Public confidence in the vaccines will be crucial to whether they will truly make a difference.
In addition to issues around supply shortage and access by developing countries to the vaccines, a concern raised by many organisations since early last year, large-scale and rapid inoculation can be messy.

Scientists are also pinning their hopes on protein subunit vaccines, a technology being used by US company Novavax and also by a team led by China CDC head Gao and Anhui Zhifei Longcom Biopharmaceutical. The technology is well proven and has been used in flu shots and hepatitis vaccines but such vaccines are difficult to design.
A candidate of a protein vaccine developed by pharmaceutical giant Sanofi and GSK must be delayed until late this year because of weak clinical data.
https://www.scmp.com/news/china/science/article/3116547/coronavirus-how-will-vaccine-advances-2020-alter-pandemic-path