Story at-a-glance
- The U.S. dietary guidelines determine what foods will be served in feeding assistance programs that touch 1 in 4 Americans every month, and have great impact on the health of the U.S. public as a whole
- By restricting healthy fat, the 2015 guidelines end up having to include higher amounts of refined grains, because those foods are fortified with nutrients you’d typically get from fattier foods
- Factors that undermine the ability to create science-based policy include catering to industry interests, and protecting professional investments and reputations
May 22, 2016 By Dr. Mercola
The 2015-2020 U.S. Dietary Guidelines were recently published,1 and while they include some positive changes, they still contain serious flaws as well. In this interview, Nina Teicholz reviews a number of them—a task for which she is particularly suited, considering she’s read the entire 571-page guidance report.
Teicholz is an investigative journalist and the author of the New York Times bestseller “The Big Fat Surprise: Why Butter, Meat & Cheese Belong in a Healthy Diet.” I previously interviewed her about that book, which delves deep into the topic of healthy versus unhealthy fats.
So, why should you care about the U.S. dietary guidelines? “They don’t affect me,” you might think.
“Here’s why they matter,” Teicholz says. “They determine what foods are in the feeding assistance programs run by the US Department of Agriculture (USDA) that touch 1 in 4 Americans every month.
Those include the National School Lunch Program (NSLP) (for many people the food that their kids are getting at school), programs for the elderly, Supplemental Nutrition Assistance Program (SNAP)...and military rations.”
Dietary Guidelines Dictate What Many Americans Eat Every Day
So while you may not peruse the dietary guidelines to influence your own eating habits, they end up directly influencing the diets of many Americans, including those with the least means to take control over their own food choices, such as those depending on food programs for their daily meals.
Moreover, when you go to your doctor, your nutritionist or dietician, the nutritional recommendations you’ll get are largely based on the dietary guidelines. If following the guidelines increases your risk of health problems, then seeking professional guidance certainly doesn’t do much good.
The guidelines even have international ramifications, as nations that don’t have the resources and scientific expertise to duplicate the process simply model their own guidance after the U.S.
The rest of the world really looks to the United States as a leader in this area, even though it’s readily apparent that the guidelines must be seriously flawed in some way, since they don’t produce very good results.
Even international organizations like the World Health Organization (WHO) and the Food and Agriculture Organization of the United Nations (FAO) follow, to a large extent, the nutritional guidance developed by the U.S.
How U.S. Dietary Guidelines Gave Rise to the Obesity Epidemic
The dietary guidelines were launched in 1980. The first guidelines were actually written by a single Senate staffer who just so happened to be heavily influenced by certain scientists, and this first edition laid the groundwork for what has turned into decades of flawed advice.
Nowadays, an expert panel of about 14 members is convened every five years to review the latest evidence and make recommendations about what should remain and what needs to be changed. Statistics reveal just how influential these guidelines actually are.
In 1965, Americans ate about 40 percent of their calories as carbohydrates and another 40 percent of their calories came from fat.
The original guidelines issued in 1980 called for a diet lower in fat and higher in carbohydrates, and by 2010, Americans had indeed brought their fat consumption down below 35 percent, and increased carbohydrates to 55 to 65 percent.
The basic advice to eat more carbs has been followed ever since. Now granted, you need carbs. But not all carbohydrates are equal. Fiber-rich carbs (mostly vegetables), are essential for good health because they break down into short-chain fatty acids in your gut, which helps make ketones and nourish your body.
They also serve as fuel for beneficial bacteria in your colon. But most people don’t eat vegetables; they eat processed carbs like grains, pasta, rice, potatoes and other starchy vegetables.
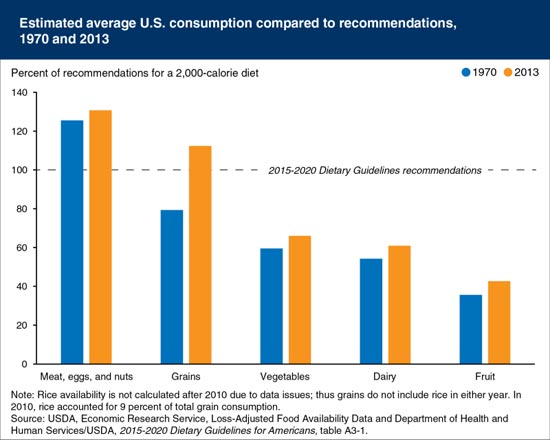
As shown in the following graph,2 fruit and vegetable consumption is trailing far behind grains, having increased only slightly since 1970, whereas grain consumption has seen the largest increase.
Fiber Versus Non-Fiber Carbs — An Important Distinction That Can Improve Your Health
I believe most people benefit by restricting the net carbs to less than 50 grams per day (i.e. total carbs minus fiber). Subtract the fiber from the total carbs, and that’s your total non-fiber carbs.
For most people, it would be a good idea to limit that to 50 grams a day. If you exercise a lot and are particularly active, you might be able to increase it to 100 grams.
Ultimately, whether it’s whole grain, refined grain, or sugar, it boils down to the same question: Does it contain fiber, and if so how much? This is the distinction that needs to be made, because until you sufficiently restrict net carbs, you’re unlikely to see a change in health outcomes.
“The one point to understand here is that there’s a large body of science showing that restricting total carbohydrates is an effective way to fight obesity, diabetes, and heart disease,” Teicholz says.
“Excessive carbohydrates, if you have too many net carbohydrates and too little fat, that diet seems to worsen heart disease risk factors. The shifting away from fat to carbohydrates over the last three and a half decades is plausibly what has provoked obesity and diabetes.
In fact, there’s a very disturbing chart that shows obesity rates in America being relatively flat and low. In the 1980’s (when the dietary guidelines came out), they just shoot up. You could say 1980 was really the beginning of the obesity epidemic, and thereafter the diabetes epidemic began. There’s a plausible correlation there to suggest that the dietary guidelines actually cause those nutrition-related conditions.”
Two Realities That Undermine the Ability to Create Science-Based Policy
Ideally, policy should be based on the best possible science. Today, the medical literature tells us that the low-fat diet has consistently been proven ineffective. There are good clinical trials and metanalyses that show saturated fats are unlikely to cause heart disease.
So why don’t the dietary guideline committees review that evidence and change their recommendations accordingly? Teicholz believes there are two major explanations for this:
1.There are major industry interests at stake. The guidelines are part of the USDA, and part of the USDA’s mission is to promote agriculture. At the same time, they have a mandate to tell people to eat less of some foods and more of others. Those two mandates conflict.
The food and agricultural industries also have the ability to influence the guidelines. As it stands, the industries benefitting from the guidelines include makers of carbohydrate-based foods, as well as the corn and soy industries, as corn and soybean oil are used in most processed foods.
The guidelines, which call for avoiding saturated fats, have led to a 91 percent increase in unsaturated fat consumption (mainly vegetables oils) over the past three decades. According to Teicholz: “The manufacturers of those are huge corporations: ADM, Unilever, Monsanto, and Bunge, and they clearly work closely with the scientists who are most influential over the guidelines.”
2.Another major factor that keeps the guidelines from changing is the professional investment that has grown out of the advice. Entire careers are at stake, should a guideline be admitted wrong and altered too dramatically.
“Many institutions have invested in this particular hypothesis about what makes people healthy,” Teicholz says. “The entire federal government invested in this hypothesis about what makes people healthy. The American Heart Association (AHA).
These giant institutions cannot be seen as flip-flopping on their public. They can’t be wrong. That prevents backing out of any advice that might be flawed. When they do, they’re really called out on it as they shouldn’t be. That’s embarrassing and difficult, and ultimately erodes the public’s confidence in our institutions.”
Contradictions and Scientifically Weak Advice Abounds
The report from the expert panel is 571 pages long. Teicholz actually read the entire report, and wrote an article about her findings for the BMJ last year.3 She notes the panel report contains a number of contradictions and recommendations that aren’t supported by the actual evidence. “It was very disappointing to see that this was the document that was guiding our national policy,” she says. Her article sparked a great deal of controversy—so much so the BMJ eventually retracted it.
“This article [was] the first high-level critique of the way the science is reviewed for the dietary guidelines and it makes a number of points,” Teicholz says. “It says that some of these reviews did not happen in a systematic way. They have their own system within the USDA called the Nutrition Evidence Library (NEL), which is supposed to do systematic reviews of the literature.
On a number of key topics, they did not use the Nutrition Evidence Library... including on unsaturated fats where there’s been a tremendous amount of new research in the last five years, and yet they did not do a systematic review of that literature. In quite a few cases, recommendations are based on what’s called the Grade III inconclusive evidence. There are three grades that they give evidence to judge its quality – Grade I, II, and III for available evidence.
There are a number of recommendations – including the vegetarian diet – based on what they consider to be Grade III evidence, which seems to be problematic to me. They are not supposed to, according to their own procedures, make recommendations based on such weak evidence. Probably one of the more controversial parts of the article was that I talked about what kinds of bias might have entered into the report.”
Strangely enough, committee members are not required to reveal their conflict of interest, which in and of itself raises questions. Despite bringing forth a number of important concerns, her article raised many angry and defensive responses. The Center for Science in the Public Interest (CSPI), which is closely allied with the government, got more than 170 scientists to sign a letter asking for a retraction of the article, based on 11 points they consider to be grievous flaws.4
“It does seem to be an effort to try to silence this article, a kind of censorship to prevent these issues from being discussed and debated as they should,” Teicholz says.
“The main point is that the dietary guidelines are clearly not working... The nicest thing you can say is that they have failed to fight obesity and diabetes. The meanest thing you could say is that they caused those conditions. The truth has to be somewhere in that range of possibilities...Scientists in this field ought to be curious. Why aren’t the guidelines working? Here’s a clue: maybe they aren’t based on good science. Take the clue and run with it—that ought to be the response to this article.”
Processed Vegetables Oils Have Done Great Harm
Unfortunately, there are very real consequences to getting the dietary guidelines wrong. One example of this is the vilification of saturated fats and the encouragement to decrease fat consumption. That left us with polyunsaturated fats, which can be healthy as we need some omega-6 fats, but not in the form of processed vegetable oils. These have likely caused more harm than the overall increase in carbohydrates.
As noted by Teicholz, the rise in heart disease in the U.S. goes in perfect lockstep with the rise in vegetable oils in the early 1920’s and 30’s. It was an unintended consequence of getting rid of saturated fats—a move partly orchestrated by the industry, which developed ways to extract oils from seeds and beans.
Today we’re dealing with another, very similar fallout. Once the FDA banned trans fats, the food industry started using interesterified fats and traditional vegetable oils, which produce extremely toxic byproducts when heated. One category called aldehydes are highly inflammatory, and may promote heart disease and Alzheimer’s.
So by not going far enough, and failing to make the recommendation to switch back to lard and other healthier fats, we may simply have jumped from the proverbial frying pan into the fire.
Saturated Fat Is Still Wrongly Vilified
The 2015-2020 dietary guidelines still recommend capping saturated fat consumption at a maximum of 10 percent of your daily calories. Personally, I eat a whole lot more than that, and there’s evidence to suggest some people may benefit from as much as 50 to 80 percent. Teicholz has done serious study in this area, and she offers the following rebuttal to those who insist saturated fat should be limited to protect your heart health:
“Saturated fats were condemned in the 1950s because they raised total cholesterol. When they could do better measurements, it shifted from total cholesterol to LDL cholesterol. But neither total nor LDL cholesterol, it turns out track very well with your heart attack risk. In other words, you’re just as likely to get a heart attack if you have high LDL as you have low LDL. That’s been shown in a number of clinical trials with thousands of people.
It turns out that, according to more reliable biomarkers – HDL cholesterol, your triglycerides, your LDL particle number, your LDL subfraction size, more up-to-date biomarkers that have now been developed that more reliably track with heart attacks – saturated fats looks perfectly good, if not healthy. In fact, saturated fats are the only food you can eat if you were to raise your HDL...
There’s also the fact that in the ‘60s and ‘70s, there were many large clinical trials on tens of thousands of people... where they took out saturated fats and replaced it with vegetable oils...reducing saturated fats down to 9 percent. In all of those trials, they could not demonstrate that reducing saturated fat reduced cardiovascular mortality. Those trials, a huge body of evidence, have basically been suppressed and ignored for decades.”
In the last five years, however, nearly a dozen systematic reviews and meta-analyses have looked at that clinical trial data, concluding that saturated fats have no adverse effect on cardiovascular mortality.
Yet the dietary guideline committee did not systematically review this evidence, even though they’re tasked with reviewing any new evidence that has emerged in the past five years. “They left a lot out, and that’s why they could come to the conclusion that the evidence against saturated fats was still strong in their view,” Teicholz says.
For the First Time, Dietary Guidelines Must Undergo Peer-Review
Interestingly, for the first time ever, Congress is getting involved. A meeting was held in October 2015, during which members of Congress asked USDA Secretary Tom Vilsack and Health and Human Services Secretary Sylvia Burwell (who are jointly responsible for the dietary guidelines) a number of questions, including: ‘Why did your experts not use the Nutrition Evidence Library like they’re supposed to?,’ ‘Why are you issuing recommendations on children when there’s no data on children?,’ and “Why are the guidelines still a one-size-fits-all recommendation?’
“That level of concern is much higher than it has been in recent history, if ever, again, because the dietary guidelines haven’t worked. Anybody can see that, so there is a high level of concern in the Congress about it,” Teicholz says. In the end, Congress mandated the first ever peer-review of the dietary guidelines by the National Academy of Medicine.
They also asked members of the 2015 Dietary Guidelines expert committee to recuse themselves from the process. It’s unclear how long it will take to complete this review, but it will certainly be interesting to see the results.
Silver Linings
While there are still many problems with the dietary guidelines, a few recommendations have shifted in the right direction. For example, for the first time ever, they now recommend limiting sugar to a maximum of 10 percent of your total calories. They also suggest reducing refined grains. Another first: coffee and alcohol were singled out as being healthy in moderate amounts.
However, even though the guidelines tell you to avoid refined grains and eat more healthy whole grains, the actual diet model distributed to all the food assistance programs show the same amount of refined grains as before—three to five servings of refined grains, and three to five servings of whole grains. Why did they do that?
Teicholz theory on this is that it has to do with fortification. Refined grains, like breakfast cereals are typically fortified, allowing them to get specific nutrients into the food supply, because, believe it or not, the dietary guidelines do not actually meet nutrient targets for vitamins and minerals. And why don’t they meet nutritional sufficiency?
“My hypothesis is because they limit saturated fats. Most the nutrient-dense foods where those are found are organ meats, meat, dairy, and eggs – that’s where you’ll find the nutrients. So bizarrely, that’s why you have to recommend Americans to eat three to five servings of refined grains every day. That’s one reason,” Teicholz says.
Why the Dietary Guidelines Are Inappropriate for Most Americans
Another positive change is the shift in focus from individual nutrients to dietary patterns. As Teicholz says, “Nobody goes to dinner and says, ‘Can I have 25 percent fat, please?’ You talk about food.”
Examples of food patterns include the vegetarian and the Mediterranean style diet. On the downside, when Teicholz analyzed the actual amount of food in these dietary patterns, the same old patterns were found again. They all consist of about 55 percent carbohydrates, 32 to 34 percent fat, and they all recommend most of the same foods.
“The issue is that people do respond very individually to diet. There are different nutritional needs for children. Women respond differently from men. The elderly have different nutritional needs. There are genetic factors that influence people’s responses. To continue with the one-size-fits-all diet seems too foolhardy and not a good kind of policy to have,” she says.
“There’s also the particular variation in the American population now, which is metabolic health. If you are obese or have diabetes, that is a sign of your intolerance to a certain kind of carbohydrates. There needs to be included in the guidelines a recommendation for those people, because who are those people?
Two-thirds of Americans are overweight or obese. More than half are pre-diabetic or diabetic. The guidelines are not for those people. So you’re talking about a policy that doesn’t address the majority of America. But there’s no big caveat that comes with the guidelines saying, “Hey America, most of these are not for most of you.”
Basic Advice: Eat Real Food
Perhaps the broadest dietary recommendation for health is simply to eat real food. Sure, people might eat more fat, but if it’s processed vegetables oils, you’ll simply get sick and die prematurely. By eating real food, as close to its natural state as possible, you’re likely to be much healthier simply because you’ll avoid a lot of processed foods.
Science actually confirms that a wide variety of diets can be healthy — provided they're based on real food, as unadulterated foods contain all the nutrients your body needs, and in far more ideal ratios than nutritional scientists can guesstimate.
Another requirement is that your diet be nutritionally sufficient and have the basic nutrients needed for life. “I think if you say eat real food that is nutritionally sufficient, that would be enough. That would narrow down your options,” Teicholz says. There are some really good databases out there that can help you determine whether or not you’re meeting your nutritional needs.
Beware that even this strategy has its shortcomings though. As noted by Teicholz: “The subtle twist is that nutrients are not all equally bioavailable from all foods. You need to eat, for example, fat-soluble vitamins with fats ... If you don’t have the vitamins, you can’t absorb the minerals.
So it’s more complicated than just simply tallying it up. But it’s a good start.” It can be especially useful for determining the ratios of nutrients in your diet, such as the percentage of protein, carbohydrates, and fat, or the ratio of saturated versus polyunsaturated fat.
For more guidance on what makes for a healthy diet, I recommend reading through my optimized nutrition plan. You may also print out my version of the food pyramid.
