As the crisis has unfolded, scientists have discovered more evidence about a strange and worrying feature of the coronavirus. While many people who become infected develop a cough, fever and loss of taste and smell, others have no symptoms at all and never realise they're carrying Covid-19.

Researchers say it's vital to understand how many are affected this way and whether "silent spreaders" are fuelling the pandemic.
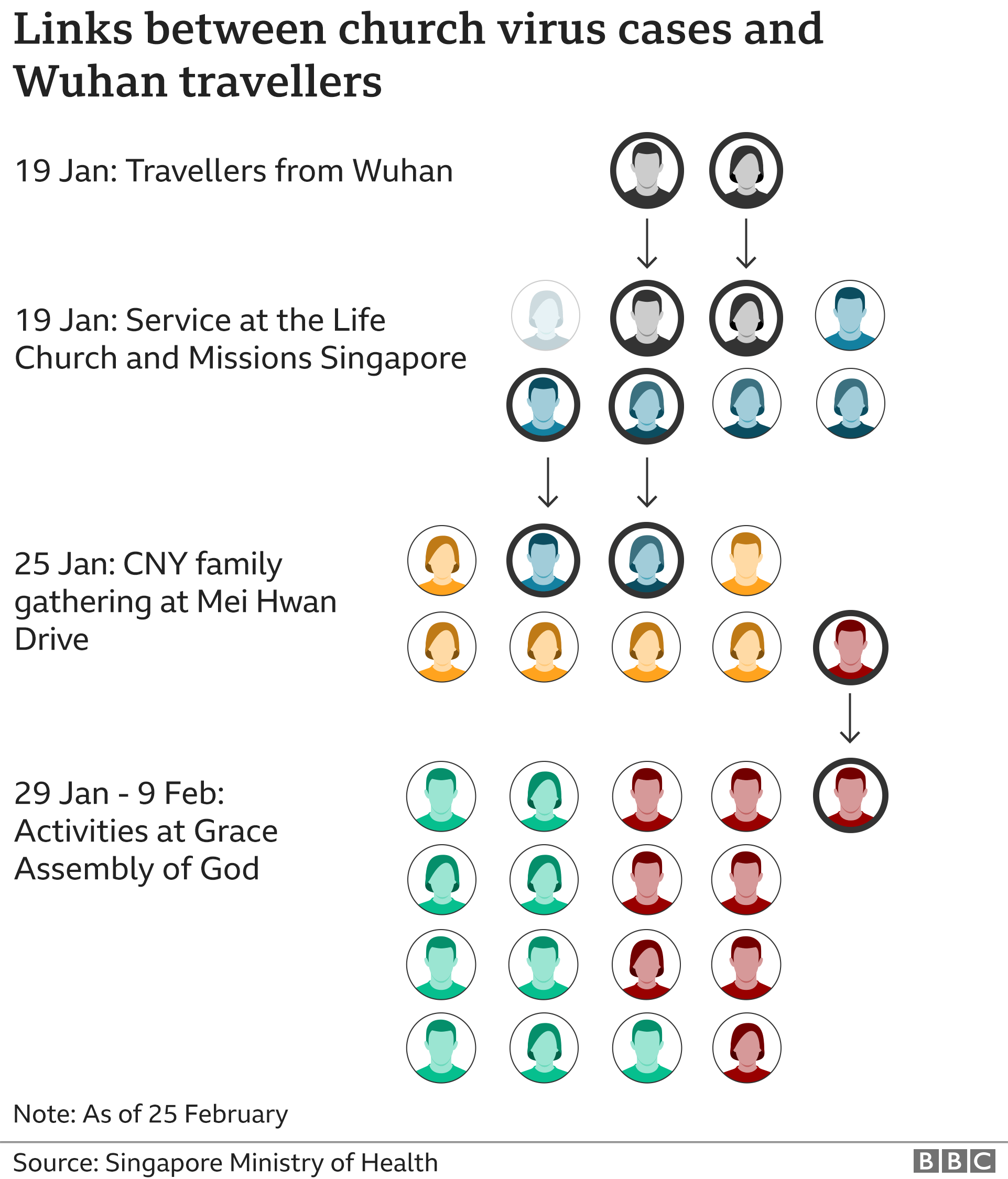
When people gathered at a church in Singapore on 19 January, no-one could have realised that the event would have global implications for the spread of coronavirus. It was a Sunday and, as usual, one of the services was being conducted in Mandarin. Among the congregation at The Life Church and Missions, on the ground floor of an office building, was a couple, both aged 56, who'd arrived that morning from China.
As they took their seats, they seemed perfectly healthy so there was no reason to think they might be carrying the virus. At that time, a persistent cough was understood to be the most distinctive feature of Covid-19 and it was seen as the most likely way to transmit it. Having no symptoms of the disease should have meant having no chance of spreading it.
The couple left as soon as the service was over. But shortly afterwards, things took a turn for the worse, and in a wholly confusing way. The wife started to become ill on January 22, followed by her husband two days later. Because they had flown in from Wuhan, the epicentre of the outbreak, that was no big surprise.
But over the following week, three local people also came down with the disease for no obvious reason, leading to one of Singapore's first and most baffling coronavirus cases. Working out what had happened would lead to a new and disturbing insight into how the virus was so successfully finding new victims.

Mobilising 'disease detectives'
"We were extremely perplexed," says Dr Vernon Lee, head of communicable diseases at Singapore's Ministry of Health. "People who didn't know one another somehow infected each other," while showing no sign of illness. This new batch of cases simply did not make sense, according to what was known about Covid-19 back then.
So Dr Lee and his fellow scientists, along with police officers and specialist disease trackers, launched an investigation, generating detailed maps showing who was where and when. This involved the very best of the process known as contact tracing - a version of which is getting under way now in the UK. It's seen as a vital system for tracking down everyone involved in an outbreak and helping to stamp it out, and Singapore is renowned for the skill and speed with which this is carried out.
 GETTY IMAGES
GETTY IMAGES
Amazingly, within a few days, investigators had spoken to no fewer than 191 members of the church and had found out that 142 of them had been there that Sunday. They quickly established that two of the Singaporeans who became infected had been at the same service as the Chinese couple.
"They could have spoken to each other, greeted each other, during the usual activities of a church service," says Dr Lee.
That was a useful start and would explain in theory how the infection could have been passed on, apart from one key factor. It did not answer the crucial question of how the virus could have been transmitted by the two Chinese people when at that stage they had shown no indication of having the disease.
And on top of that was an even greater puzzle. It was confirmed that the third Singaporean to become infected, a 52-year-old woman, had not been at the same service as the others. Instead she had attended another event in the same church later that day, so how could she have picked up the virus?

Evidence no-one expected
Investigators resorted to going through the CCTV recordings made at the church that Sunday to search for clues. And they stumbled across something completely unexpected - the woman who'd attended the later service, after the Chinese couple had left, had sat in the seats they had used several hours earlier.
Somehow, despite having no symptoms and not feeling ill, the Chinese husband and wife had managed to spread the virus. Maybe they'd had it on their hands and touched the seats, maybe their breath carried the infection and it landed on a surface, it's not clear, but the implications were huge.
For Dr Lee, piecing everything together, there was only one possible explanation - that the virus was being passed by people who had it without even realising. This was a revelation that would be relevant the world over because the central message of all public health advice on coronavirus has always been to look out for symptoms in yourself and others.
But if the virus was also being spread by people without symptoms, silently and invisibly, how could the disease be stopped? He remembers the moment, while working in his office, when the reality dawned on him. "Every time you make a scientific discovery, it is like a 'eureka' moment when you realise that this is something important that you've uncovered, through the hard work of many individuals and teams."

Spread before symptoms show
What was revealed was what's known as "pre-symptomatic transmission" where someone is unaware of being infected because the cough, fever and other classic symptoms have yet to begin.
 GETTY IMAGES
GETTY IMAGES
Along with many others, this study highlighted a critical period of 24-to-48 hours before the visible onset of the disease in which people can be highly infectious, perhaps even their most infectious.
Being aware of that is potentially invaluable, because as soon as you realise you're ill then everyone you've been in close contact with can be warned to stay at home.
That would mean that they would be isolating during the key phase of infection before their own symptoms start. But exactly how the disease can be transmitted without a cough to project droplets containing the virus is still open to debate.
One option is that simply breathing or talking to someone can do the job. If the virus is reproducing in the upper respiratory tract at that time then it's possible that some of it will emerge with each exhalation. Anyone close enough, especially indoors, could easily pick it up.
And another potential form of transmission is by touch - the virus gets onto someone's hands and they touch another person or a door handle - or a seat in a church. Whatever the route, the virus is clearly exploiting the fact that people are bound to be less vigilant if they're not aware that they might be infected.

Some people never show symptoms
This is an even more mysterious scenario, and one that scientists simply have no definitive answer to. It's one thing to know that people can be infectious before their symptoms show, quite another when they become infected but never have any sign of it.
This is what's known as being "asymptomatic" because you are a carrier of the disease but do not suffer in any way yourself. The most famous case is that of an Irish woman who was working as a cook in New York at the beginning of the last century.
 GETTY IMAGES
GETTY IMAGES
Wherever Mary Mallon was employed, in house after house, people became ill with typhoid and at least three, maybe many more, died of it, but she was completely unaffected. Eventually a connection was established and it was confirmed that she was the unwitting spreader of the disease.
Reporters dubbed her "Typhoid Mary", a label she always resented, but the authorities took no chances and kept her in confinement for 23 years until her death in 1938.

Assumptions undermined

Staff nurse Amelia Powell was shocked when she found out that she is asymptomatic. She was at work on her hospital ward at Addenbrooke's Hospital in Cambridge in April when a doctor rang to give her the result of a swab test.
She had been feeling normal and safe behind the personal protective equipment she had to wear while caring for patients with Covid-19. But suddenly all those assumptions were undermined because, to her horror, she had tested positive.
"It was a bit like hearing that someone in the family had passed, it was surreal. "I thought, 'This can't be right, not me, I'm absolutely fine,'" says 23-year-old Amelia.
She had to leave her post straightaway to go into isolation at home.


- A SIMPLE GUIDE: What are the symptoms?
- RISK AT WORK: How exposed is your job?
- HOW A VIRUS SPREADS: An explanation
- RECOVERY: How long does it take to get better?


"I was worried because I've seen the other side, with patients deteriorating very quickly with it, so I did wonder if this would happen to me." But, to her surprise, at no point did she feel unwell. "I had nothing, literally - I was exercising indoors, eating normally, sleeping normally."
At the moment it's impossible to know how many cases of infection exist but remain hidden from view.
The discovery that Amelia was infected was only revealed because she was part of a study of all the staff at her hospital. It produced the surprising result that as many as 3% of more than 1,000 people were positive while showing no symptoms at the time of the test.
An even greater proportion of asymptomatic cases was found on the Diamond Princess cruise ship which had been sailing off the coast of Japan earlier this year. Later branded "a petri dish for infection", it had around 700 cases.
Researchers found that three quarters of the people who had tested positive had no symptoms.
And at a care home in Washington state more than half the residents were positive but had no sign of the illness.

'No single reliable study'
Different studies suggest a huge range of possibilities for how many cases are asymptomatic stretching from 5% to 80% of cases. That was the conclusion of an analysis by Prof Carl Heneghan of the University of Oxford and colleagues who looked at 21 research projects.
The upshot, they said, was that "there is not a single reliable study to determine the number of asymptomatics". And they said that if the screening for Covid-19 is only carried out on people with symptoms - which has been the main focus of UK testing policy - then cases will be missed, "perhaps a lot of cases".

The risk of 'silent spreaders'
The biggest concern of Amelia, the nurse, was that she might have unwittingly transmitted the virus either to those she works with or to the patients who depend on her help.
"I don't think I passed it on because all the colleagues I work with tested negative but it was worrying to think how long I'd been positive for," she says. "But we still don't know if people who are asymptomatic are contagious or not - it's very bizarre and the information about it at the moment is minimal."
One study in China which found that the number of asymptomatic cases was actually greater than those with symptoms had a warning for the authorities. "As 'silent spreaders'," the scientists wrote, "asymptomatic carriers warrant attention as part of disease prevention and control."
 GETTY IMAGES
GETTY IMAGES
The team that studied that Diamond Princess reckoned that asymptomatic cases were likely to be less infectious than people with symptoms but even so they're estimated to have caused a significant number of cases.

The 'dark matter' of asymptomatic infection
To try to get an answer, scientists in Norwich are pushing for the population of the entire city to be tested.
"Asymptomatic cases may be the 'dark matter' of the epidemic," according to Prof Neil Hall, head of the Earlham Institute, a life science research centre, who's leading the initiative. Dark matter is the invisible substance believed to make up most of the matter in the universe, and it's yet to be identified.
Prof Hall worries that asymptomatic cases may actually be driving the pandemic, keeping it going despite public health measures. "If you have people who don't know they're ill while using public transport and health care facilities, inevitably that's going to increase transmission," he says.
"Any intervention that's only based on people coming to primary health care when they have symptoms will only deal with half the problem."
A team of scientists in California believes that not knowing who's carrying the virus without symptoms is the "Achilles Heel" of the fight against the pandemic.
 GETTY IMAGES
GETTY IMAGES
In their view, the only way to stop the disease from spreading is to find out who's infected regardless of whether they think they are or not. That was also the recommendation of MPs on the Commons Science and Technology Committee in a letter to the Prime Minister Boris Johnson.
They wrote that the risk of asymptomatic transmission has "a profound consequence for the management of the pandemic". And they said that anyone looking after vulnerable people - such as health workers or care workers - should be given regular testing.
A similar approach is being adopted on a far larger scale in the Chinese city of Wuhan, where the pandemic is thought to have begun.
As many as 6.5 million people there were tested in as little as nine days in a mass screening programme designed to detect the disease - including in those showing no symptoms.

Easing of lockdown
As lockdown measures are eased and more people start to use public transport, return to work or go shopping, getting to grips with the invisible risk matters more than ever. At the moment, there is no way of telling who among the growing crowds may be carrying the virus without knowing.
That's why governments the world over say it's essential that everyone cooperates with efforts to trace the contacts of anyone infected and then quickly self-isolates. They also advise that the best defence remains social distancing - to keep apart wherever you can. But where that isn't possible, the recommendation is to cover your face, even with a mask that's homemade.
 GETTY IMAGES
GETTY IMAGES
When the US government announced this policy, it highlighted the discoveries made in the church in Singapore back in January. The logic is that this is not about protecting yourself, it's about protecting others from you, in case you're infected but don't know it.
Many health professionals worry that masks might distract people from hand washing or social distancing, or increase the risk of contamination if they're clumsily handled. But more and more governments, most recently that of the UK, have become convinced of the benefits.
Not that face coverings will halt the pandemic on their own. But because there's still so little we know about asymptomatic transmission, almost anything is worth a try.
You may also be interested in:

When you talk to intensive care doctors across the UK, exhausted after weeks of dealing with the ravages of Covid-19, one phrase emerges time after time: "We've never seen anything like this before."
They knew a new disease was coming, and they were expecting resources to be stretched by an unknown respiratory infection which had first appeared in China at the end of last year.
"It felt in some ways like we were trying to prepare for the D-Day landings," says Barbara Miles, clinical director of intensive care at Glasgow Royal Infirmary, "with three weeks to get ready and not a great deal of knowledge about what we would be facing".
https://www.bbc.com/news/uk-52840763