Some never fully recover, and those who do often must relearn basic skills such as walking and swallowing.
By and
 |
| Diana Aguilar, 55, spent 10 days on a ventilator fighting for her life in Somerset hospital, New Jersey.Source: Aguilar family |
She was struggling to breathe, and every inch of her body ached as she felt it failing. And then came the intubation, a last-resort intervention to save her life. It’s an awful moment for each of the many thousands of patients who are estimated to have undergone the procedure.
As the cases of Covid-19 infection soar, already approaching 900,000 Americans, more and more patients are going through the same dreaded treatment. The lucky ones pull through, but their journey back to health is long and perilous. Doctors are only now learning about the challenges ahead for people who arrive at the hospital so breathless and low on oxygen that a ventilator, many believe, is all that’s standing between them and death.
“Mechanical ventilation is a life-saving intervention,” says Hassan Khouli, chair of critical care at the Cleveland Clinic in Ohio. Yet even when patients survive, “some of them will continue to be profoundly weak,” he says. “It can get to the point where they can’t perform daily activities — shaving, taking a bath, preparing a meal — to the point they could be bedridden.’’
Just a few weeks ago, when the success of social-distancing strategies was far from assured, various models estimated that the U.S., with about 63,000 of the devices available across the country, would fall dramatically and tragically short of the numbers needed. At one point, it was estimated that New York City alone may need 40,000 ventilators. Auto manufacturers agreed to work with medical-device makers to ramp up emergency production. And as makeshift hospitals sprang up in New York’s Central Park and in conference centers and gymnasiums across the country, plans were hatched to put two patients on a single ventilator to double capacity.
Now there’s good news: It appears that U.S. hospitals will need fewer than 17,000 devices to treat Covid-19 patients, according to one widely used model. What the final numbers will look like as the virus continues its march across the country is anyone’s guess. But there’s little doubt there will be thousands of ventilator survivors once the pandemic is over. And the quality of their lives is still an open question.
When Aguilar, 55, woke up in intensive care at the end of March, she found her wrists tied to the bed frame. That, she later learned, was to stop her from tearing out the tube that ran down her throat all the way to her lungs. It was connected to a mechanical ventilator that had been breathing for her for 10 days as she lay in a medically induced coma.
A nurse slowly peeled the tape off her face and, with a flick of her wrist, yanked out the tube. Aguilar had made it through the most harrowing phase of her Covid-19 gantlet.
“They were jumping and clapping, and everybody was so happy,” she says. “I didn’t know I had all these people waiting for me, waiting to see how I’d do.”
She hadn’t yet fully grasped how close she had come to death and the long odds she had just beaten. The cheers were also because many of the patients with whom she shared the ICU eventually were rolled out in body bags. Here’s why: The lungs are dynamic, delivering inhaled oxygen into the blood supply in seconds. If they aren’t working, the damage is swift. A person can go from healthy to dead in fewer than six minutes.

When Diana Aguilar was extubated and wheeled out of intensive care, she snapped a photo of her husband, Carlos Aguilar, intubated in the room beside her own.
Source: Aguilar family
Coronavirus and the inflammation it causes is like slime, clogging up the intricate system. One of the most troubling aspects is the virus’s ability to penetrate deep within the lungs, burrowing into cells and churning out viral particles. The issue isn’t just losing those cells in the lungs that are supposed to help oxygenate the body. The problem is the lungs then become the battleground for the fight, where the human immune system takes on the foreign invader. The tightly packed cells become so swollen from fluid and inflammation they stop functioning. Survivors have likened it to the sensation of drowning.
Because SARS-CoV-2 is new to the human body, the infection can trigger a massive immune response, says Christopher Petrilli, an assistant professor at NYU Langone Health in New York.
“If you have an infection, your body tries to recruit as many immune cells as it can to fight that infection,’’ he says. “While it is effective at destroying the cells that have the virus, it has the potential to damage the surrounding tissue as well.’’
That’s where a ventilator comes in.
It can be adjusted to boost oxygen, pressure and volume, pushing the air more forcefully into the lungs. But even when a patient is severely ill, some alveoli still function well. The goal is to take the pressure off the sick regions while supporting those that are still working, making sure they have the ideal amounts of oxygen and pressure so they can enrich the blood as efficiently as possible.
Though weak, Diana felt a wave of euphoria when she was free of the ventilator. But her sense of joy was short-lived. A doctor informed her that her husband was on life support in the ICU room next to hers. Diana was crushed. Had she made it this far, only to see her husband of 35 years taken away from her? The couple had been together since Diana was just 17 years old. She wasn’t about to say goodbye to him now. The following day, as she was wheeled out of intensive care, her nurse pulled her bed up beside his room to let her peer through the glass window so she could catch a glimpse of Carlos, who was now on a ventilator, too.
“I don’t know how I pulled my body to sit up, but I wanted to see him,” she says. Her cell phone felt like a brick in her weak hand, but Aguilar managed to lift it above the bed frame to snap a photo of Carlos. She blessed him before she was whisked away, exhausted.

Health-care workers celebrate as Carlos Aguilar, 64, is discharged, with 'Here Comes the Sun' blasting over the speaker system.
Source: Somerset hospital
For years, the main focus of critical-care doctors who intubate patients has been keeping them alive, fine-tuning the treatments in an effort to improve survival rates. The machines, first introduced in 1928, were initially called iron lungs and used to help polio patients breathe. Only recently have researchers learned that the biological responses to the breathing machines that kick in almost immediately often have lasting harm.
“There are a lot of other dangers when we use mechanical ventilation,’’ says Richard Lee, interim chief of pulmonary diseases and critical-care medicine at the University of California at Irvine. “We have to sedate patients for them to tolerate a mechanical breathing tube in their lungs, and the longer you are in an ICU on sedation requiring a machine, all those other things — like decreased muscle tone and strength and the risk of hospital-acquired infections — increase.’’
The risk of dying remains higher than average for at least a year after getting off a ventilator, a risk tied to both the number of days spent on the machine and other health conditions the patient had before falling sick.

Carlos Aguilar Jr., right, picks up his father, Carlos Aguilar, left, after he was discharged from Somerset hospital on April 14. Ten days earlier he picked up his mother, Diana, from the same hospital.
Source: Somerset hospital
Yet both now face the ordeal of recovering from their treatments. Fortunately, they were able to avoid the worst-case scenario, a condition known as Post-ICU syndrome that can afflict as many as half of Covid-19 patients who survive on a ventilator, says the Cleveland Clinic’s Khouli.
Hospitals are gearing up to treat these survivors, who already number in the hundreds.
Some, like SUNY Downstate Medical Center in New York, are setting up entire rehabilitation floors to help people coming off ventilators learn how to live again. Others are trying to cut back use of the device, avoiding a rush to ventilators when oxygen may be all that’s needed.
There are also devices in development to help with recovery, such as Liberate Medical’s VentFree Muscle Stimulator. It uses electrical stimulation to trigger contractions in the abdominal wall muscles, allowing patients to “exercise,” even while they are unconscious, to keep them in some semblance of shape. The goal is to help wean them off the devices faster and ultimately boost survival rates, says Chief Executive Officer Angus McLachlan.
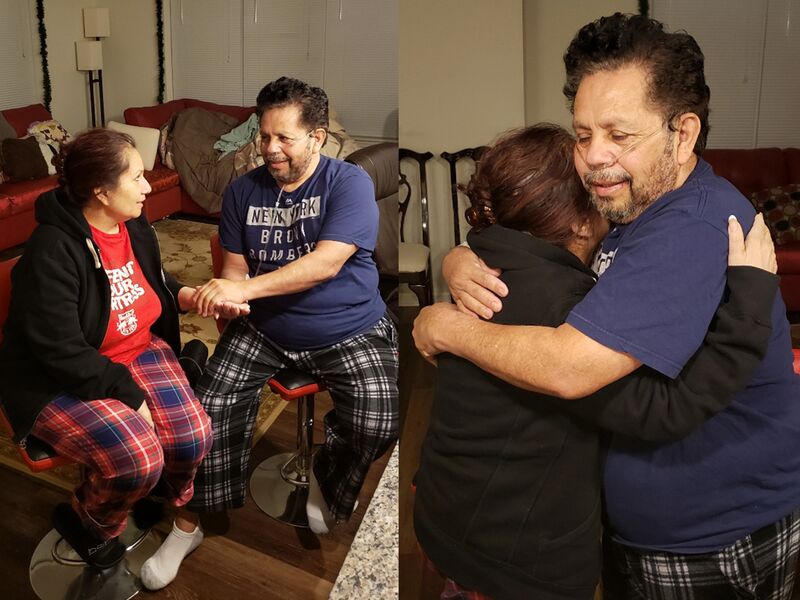
Diana and Carlos Aguilar, married 35 years, are reunited at home after both were infected with Covid-19 and intubated at Somerset hospital.
Source: Carlos Aguilar Jr.
The machines also can cause cognitive impairment, Rodricks says. A patient who worked as an accountant may have a tough time going back to work. An elderly person who was previously independent might struggle to perform daily tasks such as driving or grocery shopping. And a runner might never be able to hit the same pace again.
The recovery will be sweeter for Diana Aguilar, now that Carlos has rejoined her after being released from the hospital on April 14. So far, three weeks after her release, it’s been mercilessly slow. Diana still feels weak, with a shortness of breath and vivid nightmares that she’s back in the hospital, tied to the bed, unable to breathe. But she’s thankful.
“There is some miracle that I’m here and he’s here,” she says. “I feel like God gave us another opportunity in this life.”
https://www.bloomberg.com/news/articles/2020-04-24/life-after-ventilators-can-be-hell-for-coronavirus-survivors